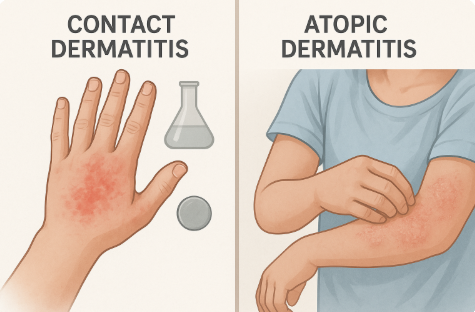
Contact Dermatitis vs Atopic Dermatitis: Understanding the Differences and Managing Flare-Ups
Have you ever wondered why your skin suddenly flares up—red, itchy, irritated, and uncomfortable? Dermatitis could be the culprit, but not all dermatitis is the same. Two of the most common types are contact dermatitis and atopic dermatitis. Understanding the difference between them can help you get closer to effective relief.
Contact Dermatitis: When Your Skin Reacts to the Outside World
Contact dermatitis happens when your skin touches something that triggers a reaction. Think of it like a sci-fi movie— the first contact sets off a chain of chaos. But in this case, it’s not aliens; it’s everyday things like harsh soaps, cleaning products, or certain metals.
There are two main types:
- Irritant contact dermatitis: This is the most common type. It occurs when a harsh substance, such as bleach, soap, or detergent, damages the skin’s outer layer. The reaction is usually immediate and localized.
- Allergic contact dermatitis: This type involves an immune response. A classic example? A nickel allergy and skin reaction. Touching jewellery with nickel can cause itching, redness, or even blisters. Poison ivy, latex, and certain cosmetics can also be triggers. You get what I mean.
Atopic Dermatitis: A Deeper, Chronic Condition
Atopic dermatitis, the other cousin, also known as eczema, is different. It usually starts from within. It’s more about what’s going on inside you. Your genetics, immune system, and skin barrier function all play a role. It often shows up as dry, itchy patches on the elbows, knees, neck, back of ears or face. While it’s more common in children, adults aren’t immune to it.
Atopic dermatitis isn’t contagious, but it is often hereditary. If eczema runs in your family, you may be more likely to experience it yourself—especially if you also have asthma or hay fever.
Similar Symptoms, Different Roots
While contact dermatitis and atopic dermatitis may both show up . These two types of dermatitis can sometimes get together and party with overlapping symptoms such as red, itchy skin, their root causes are different. However, they can coexist or even exacerbate one another. For example, someone with atopic dermatitis might also develop irritant contact dermatitis when exposed to a harsh substance due to their already weakened skin barrier.
The Role of Genetics and the Environment
Your skin is your first line of defence, but for many people with atopic dermatitis, that defence isn’t as strong as it should be. One key factor is a filaggrin mutation—a genetic defect that prevents skin cells from sticking together properly. Basically, if your skin’s missing this, it’s like leaving your front door open in a snowstorm or like missing mortar between bricks. Without it, your skin loses moisture and lets allergens in.
What so important about Filaggrin? It’s a key protein in the outermost layer of your skin (epidermis). It binds proteins and strengthens the skins barrier and retains moisture .
But it’s not all genetics. Environmental triggers—like cold weather, dry air, pollution, household cleaners, and even spicy foods—can set off flares. This is especially true when your skin is already compromised or inflamed making a genetically predisposed situation go from calm to chaos in no time.
Nickel Allergy and Skin Reaction: A Common Contact Culprit
Nickel is one of the most common allergens in allergic contact dermatitis. Found in jewellery, belt buckles, zippers, and even some electronics, it can trigger a strong skin reaction in sensitive individuals. Signs of a nickel allergy and skin reaction include redness, itching, dry patches, and sometimes fluid-filled blisters at the site of contact.
Avoiding known triggers and wearing hypoallergenic materials can make a big difference. Just knowing the usual suspects can save you a lot of grief. It’s kind of like pre-emptively breaking up with someone before the drama starts – a wise and headache-saving method.
Diagnosing and Managing Dermatitis
Getting a proper diagnosis is key to managing both types of dermatitis. For atopic dermatitis, your doctor might look at your personal and family history and examine recurring flare-up patterns.
For contact dermatitis, especially when you suspect a nickel allergy or another specific trigger, patch testing or Atopy Patch Testing (APT) can be useful. These tests expose your skin to small amounts of potential allergens and help identify what’s setting you off.
Tips for Accurate Testing:
- Avoid lotions, creams, and steroids before testing.
- Track symptoms and suspected triggers in a journal to help your doctor zero in.
Managing Dermatitis: What You Can Do
Daily management is just as important as medical treatment. Whether you’re dealing with irritant contact dermatitis or atopic dermatitis, here’s how you can reduce flare-ups:
- Use fragrance-free and gentle skincare products. Harsh soaps or perfumes can worsen symptoms.
- Moisturize regularly. Keeping your skin hydrated strengthens your barrier.
- Avoid known allergens. If nickel is a trigger, choose jewellery labelled “nickel-free.”
- Stay ahead of seasonal changes. Cold, dry air can lead to more flare-ups, so switch up your skincare accordingly.
- Don’t trust labels blindly. “Hypoallergenic” doesn’t mean allergen-free—always patch test new products before fully committing.
Final Thoughts
Whether you’re battling contact dermatitis from a known trigger like nickel, or dealing with atopic dermatitis that runs in the family, awareness is your strongest tool. By understanding the root causes and learning how to manage flare-ups, you can take back control of your skin’s health—and your comfort.

This is such an informative post — thanks for shedding light on the difference between contact and atopic dermatitis. I’ve always been curious about skin reactions to accessories. I wonder, is it true that wearing fancy jewelry (like costume pieces) instead of real gold or silver can trigger contact dermatitis?
It’s definitely something to think about, especially for those of us who love accessorizing but have sensitive skin. Thanks again for the helpful awareness tip!
This is such an informative post! I’ve personally struggled with both contact and atopic dermatitis, so I really appreciate the clear breakdown of each type. It’s fascinating how our genetics play such a significant role in skin health, yet environmental factors can also trigger flare-ups. I had no idea about the impact of filaggrin mutations—definitely makes me think about how I care for my skin!
I’ve found that keeping a symptom journal has been incredibly helpful in identifying my triggers, especially with nickel allergies. It’s like having a detective’s notebook for my skin! For anyone else dealing with similar issues, I highly recommend tracking what you come into contact with. Thanks for shedding light on such an important topic!